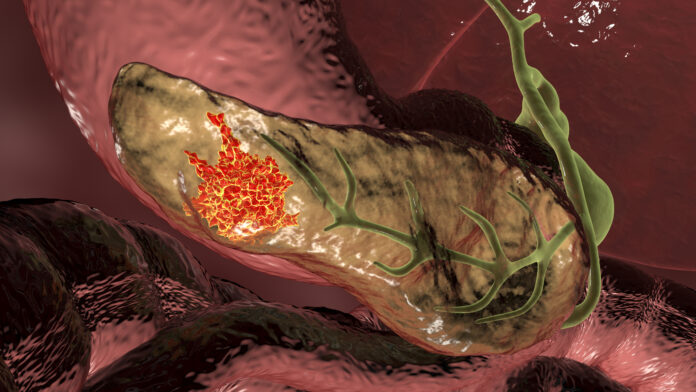
Researchers at Virginia Commonwealth University have discovered a new way of using a synthetic double-stranded RNA for the treatment of pancreatic ductal adenocarcinoma (PDAC), an aggressive type of pancreatic cancer.
As the most common form of pancreatic cancer, 95% of all pancreatic cancers are diagnosed as PDAC. It is also one of the most difficult-to-treat cancers. PDAC has a one-year survival rate of 24% and a five-year survival rate of 9%.
This poor prognosis has several reasons. Pancreatic cancer is commonly diagnosed at a late stage because symptoms only appear once the disease has progressed, and there is still a lack of early detection methods. Moreover, traditional treatments have failed to show significant effects.
Researchers are therefore looking at immunotherapeutic approaches to treat pancreatic cancer. However, the PDAC tumor microenvironment is proving tricky to navigate and remains a physical barrier to drug delivery.
In their preclinical study published in the Journal for ImmunoTherapy of Cancer, the researchers deployed a new way of delivering polyinosine-polycytidylic acid (pIC)—a synthetic double-stranded RNA—directly into the tumor cell.
“Unfortunately, clinical trials with naked pIC documented poor stability… as well as no detectable antitumor effects in melanoma and other cancers,” write the authors. Other studies, however, have suggested that “modifying pIC may provide enhanced benefit for cancer therapy.”
Based on this knowledge, the researchers used a synthetic, water-soluble polymer called polyethyleneimine (PEI) to deliver pIC directly into the cytoplasm of the tumor cell. They found that pIC combined with PEI suppressed tumor growth and induced the death of tumor cells.
“In studying this phenomenon in mice with an intact immune system, we found that it worked exceptionally well in PDAC, extending life to an amazing degree just on its own… Nothing like this has been seen before when looking at the original pIC molecule without the use of PEI or other therapeutic modalities in PDAC,” said Paul B. Fisher, co-lead of the study and a professor at Virginia Commonwealth University, in a press release.
The researchers also looked at this approach in combination with a standard chemotherapy treatment called gemcitabine. They found that the combination treatment was able to enhance the effects of pIC and PEI, resulting in the suppression of tumor growth and tumor cell death.
These results indicate that the combinational approach may have the potential to improve the survival of patients with PDAC. Furthermore, the toxicity profiles of pIC and gemcitabine are known, meaning that the approach is safe to be tested in clinical trials.
“The big picture is that this approach works, and it’s ready to go into the clinic to treat patients with pancreatic cancer,” said Fisher.
Another promising result of the study was that mice with intact immune systems that had been treated with pIC before developing cancer, showed a significantly slower eventual tumor growth. These findings suggest that pIC could even have a “protective, vaccine-like effect.” However, this area needs to be studied further, write the researchers.
“Translating discoveries that originate in the laboratory into effective therapies is a major challenge that, when accomplished, represents the ultimate achievement of basic medical research. For PDAC patients, we think there could be a light at the end of the tunnel,” Fisher concluded.













